The probability of getting pregnant is closely linked to the ovarian reserve. An evaluation of the ovarian reserve as part of an infertility evaluation is therefore recommended, especially when there are signs of difficulty in conceiving a child.
A predefined number of ovarian follicles
A reduced ovarian reserve is the leading cause of age-related female infertility. Unlike men who are able to constantly renew their sperm cells, women are born with a predefined number of eggs. A woman’s ovarian reserve (also called oocyte reserve) continues to decrease over her lifetime. The speed of deterioration of the ovarian reserve is different for every woman. For illustrative purposes, a 35-year-old woman has only about 12% of her ovarian reserve left and this percentage decreases to 3% by the age of 40.
Two methods are available to estimate a patient’s ovarian reserve: transvaginal ultrasound and a blood test.
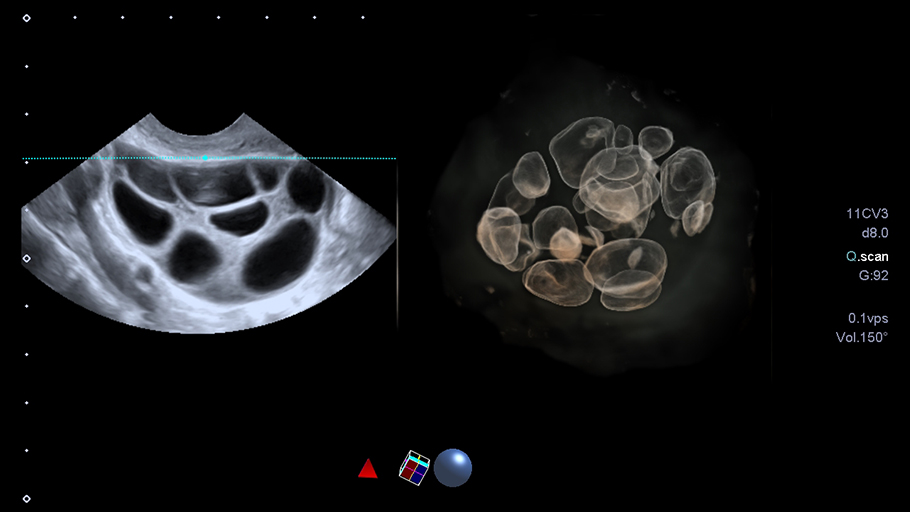
Transvaginal ultrasound
The ultrasound is done at the beginning of the cycle. The purpose of this transvaginal ultrasound is to count the follicles. Follicles are spherical in shape (tiny structures measuring 2 to 10 mm) and they are located in the ovaries. We use an transvaginal probe to get as close as possible to the ovaries.
Thanks to this technique, the image is much sharper and the 2 mm follicles are more easily visible, which allows us to count them under optimal conditions. The ultrasound cannot be done using a suprapubic ultrasound (on the belly) since the image will have a lower quality and thus, the follicles count won't be as accurate.
Before we select a follicle to enlarge and release the egg during ovulation, we count the number of antral follicles (follicles that haven't yet reached their mature stage, we also call them resting follicles) on each ovary (right and left) and we add them up. The result is the AFC (antral follicles counting) of this cycle. The antral follicles are programmed two to three months in advance to ensure the next ovulations. Based on a chart which takes into account your age, we can assess whether you are above or below the average AFC.
During this ultrasound, we conduct an overview of the uterus. We ensure there is no fibroid in the uterine cavity or polyp that could hinder the implantation of the embryo.
Blood test
A blood test is performed at the start of the cycle which includes the dosage of several hormones:
- Antimüllerian Hormone (AMH): This hormone, compared to the others we measure, does not fluctuate according to the phase of the menstrual cycle but rather according to the woman's age. It is high at puberty, and decreases until menopause. Thanks to this dosage, we can have a good idea of the state of the ovarian reserve. The level of this hormone is directly linked to the stock of oocytes. If it is low, the reserve will be low. However, if the rate is high, we can expect polycystic ovary syndrome.
- Follicle stimulating hormone (FSH): This hormone is used for the maturation and growth of follicles. If this rate is clearly high, there could be ovarian failure. If it is low, the problem may be related to the pituitary gland (other tests will be suggested in this case).
- Estradiol: secreted by the ovaries, it plays an important role in the regulation of menstrual cycles as well as in the quality of ovarian secretion. If FSH is high and estradiol is low, we can suspect early menopause.